AI and Automation in Medical Claims Processing
AI and Automation in Medical Claims Processing
AI and Automation in Medical Claims Processing
AI and Automation in Medical Claims Processing
Anant Sharma
Anant Sharma
Anant Sharma
AI and Automation in Medical Claims Processing
In the healthcare industry, the efficiency and accuracy of medical claims processing are crucial for ensuring timely reimbursements and reducing administrative costs. However, traditional methods of handling claims are often slow, error-prone, and costly, impacting healthcare providers and patients.
With the growing volume of claims and increasing pressure to streamline operations, AI and automation have become game-changing solutions. By harnessing the power of AI in healthcare claims processing, organizations can dramatically improve accuracy, speed, and cost-effectiveness while also reducing human error and fraud.
In this blog, we will dive into how AI and automation are transforming medical claims processing and why adopting these technologies is essential for the future of healthcare.
How AI Voice Bots Address the Healthcare Claims Process?
AI and automation are changing medical claims processing by streamlining the workflow, reducing human error, and accelerating reimbursement timelines. Traditionally, claims processors manually reviewed medical claims. They had to check for compliance with insurance policies, verify service codes, and ensure the claims were valid. This process is time-consuming and prone to inaccuracies.
AI algorithms can analyze claims data much faster than humans, identifying inconsistencies, flagging errors, and even predicting the possibility of a claim payment based on historical data. Automation also plays a key role by taking over repetitive tasks, such as data entry, claims verification, and status updates. This helps reduce the overall cycle time of claims processing while increasing efficiency across the board.
By utilizing AI in healthcare claims processing, you can significantly reduce the workload on human staff, improve claims processing accuracy, and enhance the overall customer experience. Automation can also help reduce fraud by flagging suspicious claims and ensuring all required documentation is complete before submission. These advancements are driving operational efficiencies in the claims processing world.
Drawbacks of Manual Claims Processes
Despite significant technological advancements, many healthcare organizations continue to rely on manual processes for handling medical claims. While these methods may have been sufficient in the past, they now present several serious drawbacks that can negatively impact both you and your patients. Here are some of the major disadvantages of manual claims processes:
Increased Risk of Errors and Delays
Manual claims processing often involves a lot of paperwork, making it prone to human error. Misfiled documents, incorrect coding, or incomplete data can lead to rejected or delayed claims. These errors extend reimbursement cycles and increase administrative costs, ultimately affecting your organization's financial health and the patient experience.
Labor-Intensive and Time-Consuming
The manual review process is highly time-consuming. Claims processors must verify eligibility, check for duplicates, and ensure compliance with policies. These tasks demand significant time and effort, which leaves less room for addressing more complex cases. With the increasing volume of healthcare claims, this manual approach becomes less sustainable and further prolongs the claim resolution process.
Risk of Financial Loss and Discontent
Human error is inevitable in a labor-intensive process like manual claims management. Incorrect coding, billing errors, and missed deadlines can result in revenue loss and delayed payments. These mistakes can create dissatisfaction among patients and healthcare providers, causing frustration and hindering relationships.
Unsuitability for Growing Claim Volumes
As healthcare claims continue to grow in both volume and complexity, relying on manual processes becomes increasingly inefficient. You may struggle to keep up with the sheer volume of claims, leading to longer processing times and reduced overall effectiveness.
To address these challenges, AI tools like Rifa AI can streamline and automate many manual tasks involved in claims processing. AI solutions enable faster reimbursements and more efficient workflows by significantly reducing human error and improving overall accuracy. This enhances operational efficiency and ensures you can focus on more complex tasks requiring human oversight, improving patient care and organizational performance.
Key Benefits of AI and Automation in Healthcare Claims Management
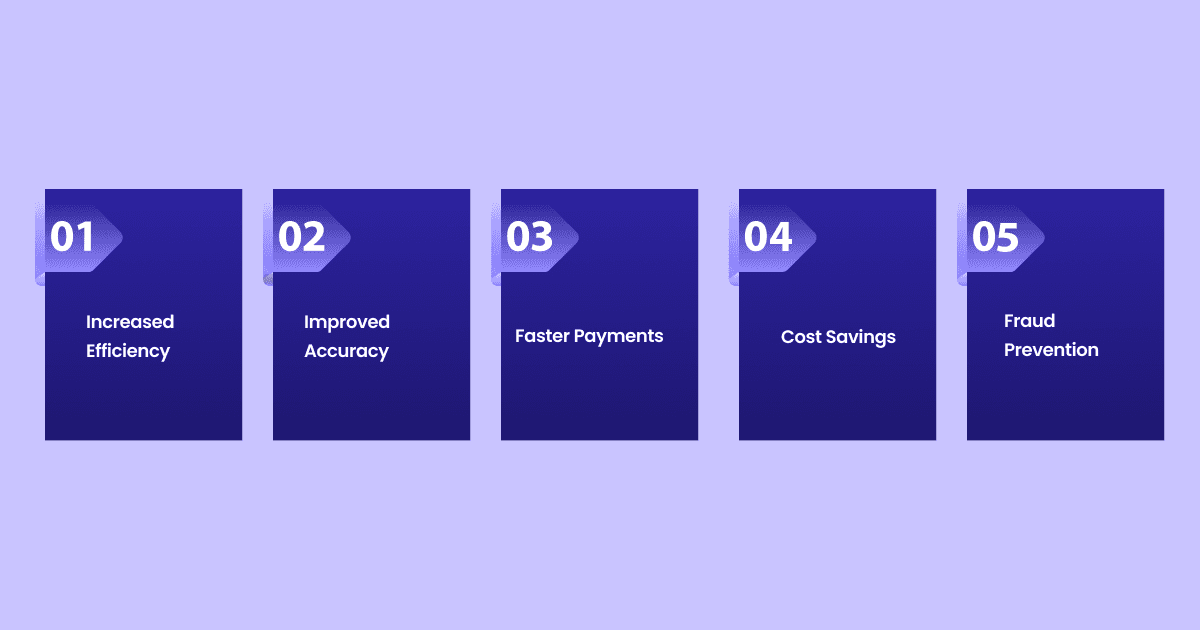
The integration of AI into healthcare claims management brings a host of benefits. Not only does it enhance the accuracy of claims processing, but it also provides faster turnaround times and reduced administrative costs. Here are the key advantages:
Increased Efficiency: AI can process large volumes of claims at a fraction of the time it takes human employees. Automated systems like Rifa AI can handle tasks such as claim data entry, document validation, and status updates, drastically improving operational efficiency.
Improved Accuracy: AI algorithms analyze claims data, checking for errors in coding, billing, and eligibility. These systems can automatically flag potential issues, which helps reduce the number of rejected or denied claims due to human employees overlooking some details by mistake. Rifa AI can seamlessly update and migrate patient health records accurately.
Faster Payments: By automating repetitive tasks, AI expedites the claims review process, enabling faster claim approvals and, ultimately, quicker payments. This can benefit you by improving cash flow and reducing administrative overhead.
Cost Savings: Automation reduces the need for large teams of claims processors, leading to lower labor costs. It also minimizes the risk of overpayments or underpayments due to manual errors, which can have significant financial repercussions.
Fraud Prevention: AI can spot patterns in claims data that indicate fraud, helping to detect and prevent fraudulent claims before they occur. This is particularly important in healthcare, where fraudulent billing can result in millions of dollars in losses.
Supercharge your debt collection with Rifa's AI automation: streamline 70% of workflows, achieve 99% accuracy, and save over 200 hours weekly—no API integration needed. Deploy in days and slash costs by up to 70%. Ready for transformation? Let Rifa AI lead the way to success.
Applications of AI Automated Healthcare Claims Process
Several healthcare organizations are already experiencing the benefits of AI and automation in their claims processing systems. These technologies can help you improve efficiency, reduce errors, and speed up claim approvals. Here are some specific applications of AI in automated healthcare claims processing that can directly benefit your organization:
Natural Language Processing (NLP) for Accurate Claim Review: AI systems use NLP technology to analyze unstructured data in medical records. This allows you to review clinical documentation more accurately, ensuring that submitted claims have the correct coding and billing information. You can significantly reduce errors from manual data entry with NLP, improving the overall accuracy of claims processing.
Automated Claim Adjudication: AI algorithms can evaluate the eligibility of a claim by cross-referencing it against the patient’s insurance policy and other relevant data. This process helps determine the claim validity, additional documentation requirements, or if it needs further review. By automating these tasks, you can speed up claim processing, respond to claimants more efficiently, and reduce administrative delays.
Predictive Analytics for Denial Prevention: AI can use predictive analytics to forecast claim denials based on historical data and patterns. This allows you to address issues proactively before submitting a claim, minimizing the chances of rejections and reducing administrative burdens associated with appeals and resubmissions.
Fraud Detection and Prevention: AI-powered tools can analyze claims data in real-time to detect potential fraud by identifying irregularities and suspicious patterns. This can help prevent the processing of fraudulent claims, saving your organization money and protecting providers and patients from financial losses.
Automated Data Entry and Verification: AI systems, like Rifa AI, can automatically extract and verify data from various sources, such as patient records, billing information, and insurance policies. This eliminates the need for manual data entry, which is time-consuming and error-prone, leading to faster processing times and reduced chances of mistakes.
Smart Routing for Complex Claims: AI can help route complex claims to the appropriate specialists or teams based on predefined criteria. This ensures that only the most qualified individuals handle high-priority or complex cases, improving the speed and accuracy of these claim reviews.
Enhancing Revenue Cycle Management with AI Voice Bots
Artificial intelligence (AI) is revolutionizing healthcare revenue cycle management (RCM) by automating tasks, improving accuracy, and providing valuable insights. AI-powered solutions can streamline processes such as patient registration, eligibility verification, coding, billing, and claims processing. Rifa AI is pivotal in RCM because it ensures accurate document verification and improves reimbursement strategies.
Automation reduces manual errors, accelerates workflows, and frees up staff to focus on more complex tasks. AI algorithms can also analyze vast amounts of data to identify patterns, predict denials, and optimize reimbursement strategies. This improves healthcare providers' financial performance.
Furthermore, AI enhances patient engagement and satisfaction. AI-powered voice bots can answer patient inquiries, estimate costs, and offer personalized payment options. By improving communication and transparency, AI contributes to a positive patient experience. Additionally, AI helps detect fraud and prevent revenue leakage, ensuring financial integrity. With its ability to automate, analyze, and optimize, AI is transforming RCM, enabling you to improve efficiency, increase revenue, and enhance patient care.
Steps to Implement AI Voice Bots in Claims Management
Implementing AI in healthcare claims management involves several steps, such as:
Step 1: You must assess the patient's claims process to identify pain points that automation can improve. This includes evaluating the types of claims they handle, the volume of claims, and the specific areas where errors or inefficiencies occur.
Step 2: Once you identify the key areas for improvement, the next step is to choose the right AI technology. This might include selecting AI tools for data extraction, automated decision-making, or predictive analytics. The chosen tools should integrate smoothly with existing claims management software to ensure a seamless transition.
Step 3: You must train your staff to work with the new system after selecting the appropriate technology. This ensures that your employees understand how AI and automation work and how to utilize these tools for optimal results. Continuous monitoring and improvement of the system will be necessary to ensure it delivers the desired outcomes.
Implementing AI in claims management requires careful planning, including assessing processes, choosing the right technology, and training staff. With proper integration, AI tools like Rifa AI can accelerate reimbursements, leading to better financial outcomes and patient satisfaction. These steps can help position your organization for success in healthcare.
Challenges in Claims Management
While AI and automation offer tremendous benefits for improving claims management, their integration into existing systems comes with several challenges. You must address these challenges carefully to ensure the successful implementation and long-term viability of AI-powered solutions.
High Implementation Costs
One of the primary challenges in transitioning from manual to automated claims processing is the requirement of significant financial investment. Integrating AI systems involves purchasing advanced technology and investing in training staff to use these systems effectively. This upfront cost can be substantial for your healthcare organization, and the return on investment may take time to materialize. However, once implemented, AI can reduce long-term operational costs and improve efficiency, making the initial investment worthwhile.
Resistance From Staff
The shift to automated systems may face resistance from staff unfamiliar with AI technology or fearing job displacement. Many employees may feel uncertain about their roles as automation takes over repetitive tasks. It’s crucial to manage this transition effectively, offering training and clear communication to help staff understand how AI can support their work rather than replace them. By emphasizing AI's value in streamlining workflows and allowing staff to focus on more complex tasks, you can mitigate resistance and foster a positive adoption of new technologies.
Data Security Concerns
As healthcare organizations increasingly rely on AI-driven solutions, they handle vast amounts of sensitive patient data. This raises critical concerns regarding data security and patient confidentiality. With more automated systems in place, the risk of data breaches or unauthorized access increases.
Ensuring that AI systems comply with stringent privacy regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), is essential to safeguard patient information. To protect patient data throughout the claims processing cycle, you must implement robust security measures, including encryption and access controls.
Data Quality and Accuracy
AI and automation systems are only as effective as the data fed. If the input data is inaccurate, incomplete, or inconsistent, it can lead to incorrect outcomes, such as rejected claims or delayed payments. Healthcare organizations must ensure that the data entered into AI systems is of high quality. This means implementing strict protocols for data entry, regular audits, and maintaining clear documentation to ensure that the AI system has accurate, up-to-date information to work with.
To overcome these challenges, you should take a phased approach to AI implementation. This involves investing in comprehensive training for staff, ensuring strict compliance with privacy regulations, and continuously monitoring data quality. You can fully utilize AI's potential in claims management by addressing these obstacles upfront and proactively managing the transition while minimizing risks and challenges.
Enhance your debt collection with Rifa AI: automate 70% of your procedures, minimize human error, and ensure real-time data accuracy. Our advanced encryption safeguards sensitive financial data, and we comply with regulations like GDPR. Benefit from predictive analytics to optimize compliance and collections. Transform your processes, reduce costs, and achieve near-perfect accuracy in just days with Rifa AI.
Conclusion
Integrating AI and automation into healthcare claims processing represents a significant leap forward for the industry. By addressing the inefficiencies and limitations of manual claims processing, AI in healthcare claims processing improves accuracy, speeds up reimbursements, and helps prevent fraud.
You can adopt these technologies, which will improve claims management processes and put them in a better position for the future of healthcare finance. The time to embrace AI in claims processing is now, and the rewards are too great to ignore.
Rifa AI offers an efficient, cost-effective, and personalized solution to streamline your collections and improve customer satisfaction. With real-time data processing, seamless omnichannel integration, and a fully compliant, automated system, Rifa AI is your trusted partner in debt recovery and other financial operations.
Consider that over 1 million accounts have outstanding credit card debt. Manual workflows were only 60% accurate, and API integrations for automation would take months. Rifa AI addresses these challenges head-on. Don’t wait—experience the future of debt collection today. Schedule a demo to learn how Rifa AI can revolutionize your financial operations and lead to significant cost savings.
AI and Automation in Medical Claims Processing
In the healthcare industry, the efficiency and accuracy of medical claims processing are crucial for ensuring timely reimbursements and reducing administrative costs. However, traditional methods of handling claims are often slow, error-prone, and costly, impacting healthcare providers and patients.
With the growing volume of claims and increasing pressure to streamline operations, AI and automation have become game-changing solutions. By harnessing the power of AI in healthcare claims processing, organizations can dramatically improve accuracy, speed, and cost-effectiveness while also reducing human error and fraud.
In this blog, we will dive into how AI and automation are transforming medical claims processing and why adopting these technologies is essential for the future of healthcare.
How AI Voice Bots Address the Healthcare Claims Process?
AI and automation are changing medical claims processing by streamlining the workflow, reducing human error, and accelerating reimbursement timelines. Traditionally, claims processors manually reviewed medical claims. They had to check for compliance with insurance policies, verify service codes, and ensure the claims were valid. This process is time-consuming and prone to inaccuracies.
AI algorithms can analyze claims data much faster than humans, identifying inconsistencies, flagging errors, and even predicting the possibility of a claim payment based on historical data. Automation also plays a key role by taking over repetitive tasks, such as data entry, claims verification, and status updates. This helps reduce the overall cycle time of claims processing while increasing efficiency across the board.
By utilizing AI in healthcare claims processing, you can significantly reduce the workload on human staff, improve claims processing accuracy, and enhance the overall customer experience. Automation can also help reduce fraud by flagging suspicious claims and ensuring all required documentation is complete before submission. These advancements are driving operational efficiencies in the claims processing world.
Drawbacks of Manual Claims Processes
Despite significant technological advancements, many healthcare organizations continue to rely on manual processes for handling medical claims. While these methods may have been sufficient in the past, they now present several serious drawbacks that can negatively impact both you and your patients. Here are some of the major disadvantages of manual claims processes:
Increased Risk of Errors and Delays
Manual claims processing often involves a lot of paperwork, making it prone to human error. Misfiled documents, incorrect coding, or incomplete data can lead to rejected or delayed claims. These errors extend reimbursement cycles and increase administrative costs, ultimately affecting your organization's financial health and the patient experience.
Labor-Intensive and Time-Consuming
The manual review process is highly time-consuming. Claims processors must verify eligibility, check for duplicates, and ensure compliance with policies. These tasks demand significant time and effort, which leaves less room for addressing more complex cases. With the increasing volume of healthcare claims, this manual approach becomes less sustainable and further prolongs the claim resolution process.
Risk of Financial Loss and Discontent
Human error is inevitable in a labor-intensive process like manual claims management. Incorrect coding, billing errors, and missed deadlines can result in revenue loss and delayed payments. These mistakes can create dissatisfaction among patients and healthcare providers, causing frustration and hindering relationships.
Unsuitability for Growing Claim Volumes
As healthcare claims continue to grow in both volume and complexity, relying on manual processes becomes increasingly inefficient. You may struggle to keep up with the sheer volume of claims, leading to longer processing times and reduced overall effectiveness.
To address these challenges, AI tools like Rifa AI can streamline and automate many manual tasks involved in claims processing. AI solutions enable faster reimbursements and more efficient workflows by significantly reducing human error and improving overall accuracy. This enhances operational efficiency and ensures you can focus on more complex tasks requiring human oversight, improving patient care and organizational performance.
Key Benefits of AI and Automation in Healthcare Claims Management
The integration of AI into healthcare claims management brings a host of benefits. Not only does it enhance the accuracy of claims processing, but it also provides faster turnaround times and reduced administrative costs. Here are the key advantages:
Increased Efficiency: AI can process large volumes of claims at a fraction of the time it takes human employees. Automated systems like Rifa AI can handle tasks such as claim data entry, document validation, and status updates, drastically improving operational efficiency.
Improved Accuracy: AI algorithms analyze claims data, checking for errors in coding, billing, and eligibility. These systems can automatically flag potential issues, which helps reduce the number of rejected or denied claims due to human employees overlooking some details by mistake. Rifa AI can seamlessly update and migrate patient health records accurately.
Faster Payments: By automating repetitive tasks, AI expedites the claims review process, enabling faster claim approvals and, ultimately, quicker payments. This can benefit you by improving cash flow and reducing administrative overhead.
Cost Savings: Automation reduces the need for large teams of claims processors, leading to lower labor costs. It also minimizes the risk of overpayments or underpayments due to manual errors, which can have significant financial repercussions.
Fraud Prevention: AI can spot patterns in claims data that indicate fraud, helping to detect and prevent fraudulent claims before they occur. This is particularly important in healthcare, where fraudulent billing can result in millions of dollars in losses.
Supercharge your debt collection with Rifa's AI automation: streamline 70% of workflows, achieve 99% accuracy, and save over 200 hours weekly—no API integration needed. Deploy in days and slash costs by up to 70%. Ready for transformation? Let Rifa AI lead the way to success.
Applications of AI Automated Healthcare Claims Process
Several healthcare organizations are already experiencing the benefits of AI and automation in their claims processing systems. These technologies can help you improve efficiency, reduce errors, and speed up claim approvals. Here are some specific applications of AI in automated healthcare claims processing that can directly benefit your organization:
Natural Language Processing (NLP) for Accurate Claim Review: AI systems use NLP technology to analyze unstructured data in medical records. This allows you to review clinical documentation more accurately, ensuring that submitted claims have the correct coding and billing information. You can significantly reduce errors from manual data entry with NLP, improving the overall accuracy of claims processing.
Automated Claim Adjudication: AI algorithms can evaluate the eligibility of a claim by cross-referencing it against the patient’s insurance policy and other relevant data. This process helps determine the claim validity, additional documentation requirements, or if it needs further review. By automating these tasks, you can speed up claim processing, respond to claimants more efficiently, and reduce administrative delays.
Predictive Analytics for Denial Prevention: AI can use predictive analytics to forecast claim denials based on historical data and patterns. This allows you to address issues proactively before submitting a claim, minimizing the chances of rejections and reducing administrative burdens associated with appeals and resubmissions.
Fraud Detection and Prevention: AI-powered tools can analyze claims data in real-time to detect potential fraud by identifying irregularities and suspicious patterns. This can help prevent the processing of fraudulent claims, saving your organization money and protecting providers and patients from financial losses.
Automated Data Entry and Verification: AI systems, like Rifa AI, can automatically extract and verify data from various sources, such as patient records, billing information, and insurance policies. This eliminates the need for manual data entry, which is time-consuming and error-prone, leading to faster processing times and reduced chances of mistakes.
Smart Routing for Complex Claims: AI can help route complex claims to the appropriate specialists or teams based on predefined criteria. This ensures that only the most qualified individuals handle high-priority or complex cases, improving the speed and accuracy of these claim reviews.
Enhancing Revenue Cycle Management with AI Voice Bots
Artificial intelligence (AI) is revolutionizing healthcare revenue cycle management (RCM) by automating tasks, improving accuracy, and providing valuable insights. AI-powered solutions can streamline processes such as patient registration, eligibility verification, coding, billing, and claims processing. Rifa AI is pivotal in RCM because it ensures accurate document verification and improves reimbursement strategies.
Automation reduces manual errors, accelerates workflows, and frees up staff to focus on more complex tasks. AI algorithms can also analyze vast amounts of data to identify patterns, predict denials, and optimize reimbursement strategies. This improves healthcare providers' financial performance.
Furthermore, AI enhances patient engagement and satisfaction. AI-powered voice bots can answer patient inquiries, estimate costs, and offer personalized payment options. By improving communication and transparency, AI contributes to a positive patient experience. Additionally, AI helps detect fraud and prevent revenue leakage, ensuring financial integrity. With its ability to automate, analyze, and optimize, AI is transforming RCM, enabling you to improve efficiency, increase revenue, and enhance patient care.
Steps to Implement AI Voice Bots in Claims Management
Implementing AI in healthcare claims management involves several steps, such as:
Step 1: You must assess the patient's claims process to identify pain points that automation can improve. This includes evaluating the types of claims they handle, the volume of claims, and the specific areas where errors or inefficiencies occur.
Step 2: Once you identify the key areas for improvement, the next step is to choose the right AI technology. This might include selecting AI tools for data extraction, automated decision-making, or predictive analytics. The chosen tools should integrate smoothly with existing claims management software to ensure a seamless transition.
Step 3: You must train your staff to work with the new system after selecting the appropriate technology. This ensures that your employees understand how AI and automation work and how to utilize these tools for optimal results. Continuous monitoring and improvement of the system will be necessary to ensure it delivers the desired outcomes.
Implementing AI in claims management requires careful planning, including assessing processes, choosing the right technology, and training staff. With proper integration, AI tools like Rifa AI can accelerate reimbursements, leading to better financial outcomes and patient satisfaction. These steps can help position your organization for success in healthcare.
Challenges in Claims Management
While AI and automation offer tremendous benefits for improving claims management, their integration into existing systems comes with several challenges. You must address these challenges carefully to ensure the successful implementation and long-term viability of AI-powered solutions.
High Implementation Costs
One of the primary challenges in transitioning from manual to automated claims processing is the requirement of significant financial investment. Integrating AI systems involves purchasing advanced technology and investing in training staff to use these systems effectively. This upfront cost can be substantial for your healthcare organization, and the return on investment may take time to materialize. However, once implemented, AI can reduce long-term operational costs and improve efficiency, making the initial investment worthwhile.
Resistance From Staff
The shift to automated systems may face resistance from staff unfamiliar with AI technology or fearing job displacement. Many employees may feel uncertain about their roles as automation takes over repetitive tasks. It’s crucial to manage this transition effectively, offering training and clear communication to help staff understand how AI can support their work rather than replace them. By emphasizing AI's value in streamlining workflows and allowing staff to focus on more complex tasks, you can mitigate resistance and foster a positive adoption of new technologies.
Data Security Concerns
As healthcare organizations increasingly rely on AI-driven solutions, they handle vast amounts of sensitive patient data. This raises critical concerns regarding data security and patient confidentiality. With more automated systems in place, the risk of data breaches or unauthorized access increases.
Ensuring that AI systems comply with stringent privacy regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), is essential to safeguard patient information. To protect patient data throughout the claims processing cycle, you must implement robust security measures, including encryption and access controls.
Data Quality and Accuracy
AI and automation systems are only as effective as the data fed. If the input data is inaccurate, incomplete, or inconsistent, it can lead to incorrect outcomes, such as rejected claims or delayed payments. Healthcare organizations must ensure that the data entered into AI systems is of high quality. This means implementing strict protocols for data entry, regular audits, and maintaining clear documentation to ensure that the AI system has accurate, up-to-date information to work with.
To overcome these challenges, you should take a phased approach to AI implementation. This involves investing in comprehensive training for staff, ensuring strict compliance with privacy regulations, and continuously monitoring data quality. You can fully utilize AI's potential in claims management by addressing these obstacles upfront and proactively managing the transition while minimizing risks and challenges.
Enhance your debt collection with Rifa AI: automate 70% of your procedures, minimize human error, and ensure real-time data accuracy. Our advanced encryption safeguards sensitive financial data, and we comply with regulations like GDPR. Benefit from predictive analytics to optimize compliance and collections. Transform your processes, reduce costs, and achieve near-perfect accuracy in just days with Rifa AI.
Conclusion
Integrating AI and automation into healthcare claims processing represents a significant leap forward for the industry. By addressing the inefficiencies and limitations of manual claims processing, AI in healthcare claims processing improves accuracy, speeds up reimbursements, and helps prevent fraud.
You can adopt these technologies, which will improve claims management processes and put them in a better position for the future of healthcare finance. The time to embrace AI in claims processing is now, and the rewards are too great to ignore.
Rifa AI offers an efficient, cost-effective, and personalized solution to streamline your collections and improve customer satisfaction. With real-time data processing, seamless omnichannel integration, and a fully compliant, automated system, Rifa AI is your trusted partner in debt recovery and other financial operations.
Consider that over 1 million accounts have outstanding credit card debt. Manual workflows were only 60% accurate, and API integrations for automation would take months. Rifa AI addresses these challenges head-on. Don’t wait—experience the future of debt collection today. Schedule a demo to learn how Rifa AI can revolutionize your financial operations and lead to significant cost savings.
Feb 25, 2025
Feb 25, 2025
Feb 25, 2025

